Mpox, previously known as Monkeypox, is a rare but concerning disease that has gained attention due to recent outbreaks. Understanding Mpox is crucial for effective prevention, timely treatment, and overall public health. This article delves into what Mpox is, its symptoms, available treatment options, and strategies to stay safe.
What Is Mpox?

Mpox is an infectious disease caused by the Monkeypox virus, a member of the Orthopoxvirus genus, which also includes the viruses responsible for smallpox and cowpox. Originally identified in laboratory monkeys in 1958, the virus predominantly affects rodents and primates in Central and West Africa, with occasional human infections. The disease first appeared in humans in the Democratic Republic of the Congo (DRC) in 1970.
Monkeypox is similar to smallpox but generally less severe. Its symptoms and transmission methods have prompted global health organizations to pay closer attention, especially with recent cases spreading beyond endemic regions.
Causes of Mpox
Virus Overview
The Monkeypox virus is a zoonotic pathogen, meaning it primarily infects animals but can be transmitted to humans. The virus is characterized by its double-stranded DNA and is capable of causing illness in both humans and animals.
Transmission Methods
- Human-to-Human Transmission: Mpox can spread through close contact with infected individuals, particularly via respiratory droplets, bodily fluids, or contaminated materials such as bedding and clothing.
- Animal-to-Human Transmission: People can contract the virus from handling infected animals or consuming undercooked meat. Rodents and primates are the primary animal hosts, with human cases often linked to interactions with these animals in endemic areas.
- Environmental Contamination: The virus can persist in the environment, particularly in areas contaminated by infected animals or humans, although this mode of transmission is less common.
Symptoms of Mpox
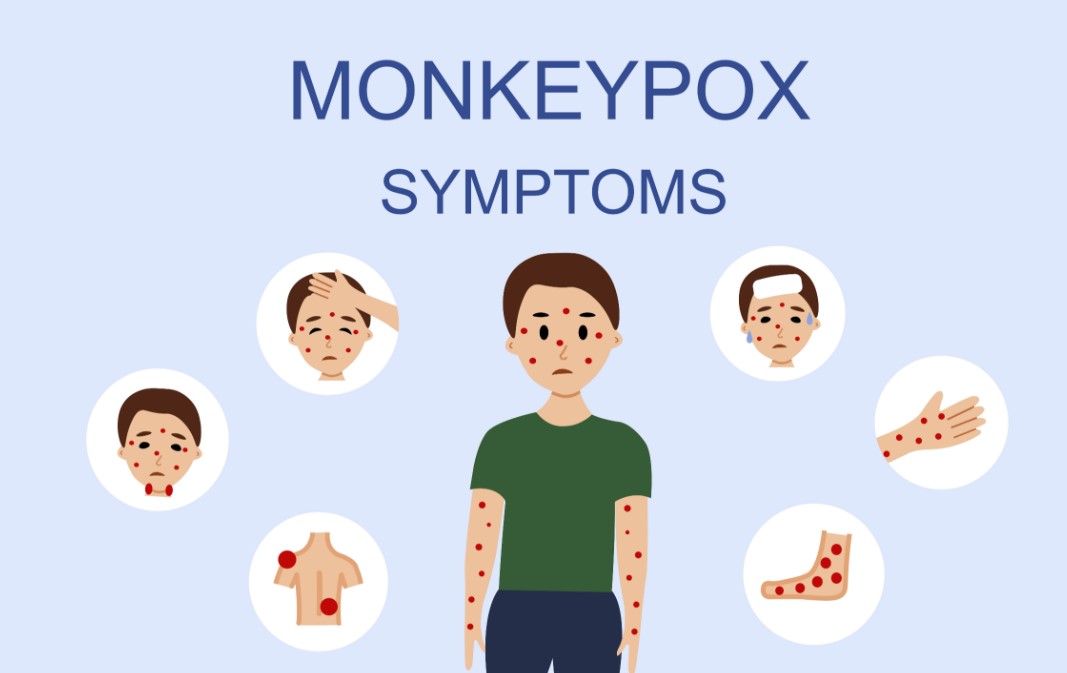
Early Symptoms
The onset of Mpox is marked by flu-like symptoms, which typically appear within 5 to 21 days after exposure to the virus. These early symptoms include:
- Fever
- Headache
- Muscle aches
- Backache
- Swollen lymph nodes
- Chills and exhaustion
These initial signs may resemble other viral infections, making early detection challenging.
Progression of the Disease
Following the flu-like symptoms, a distinctive rash develops. The rash typically begins on the face and subsequently extends to other areas of the body. It progresses through several stages:
- Macules: Flat, discolored spots on the skin.
- Papules: Raised bumps that may be itchy.
- Vesicles: Fluid-filled blisters.
- Pustules: Pus-filled lesions.
- Scabs: Crusts that eventually fall off as the skin heals.
The rash typically lasts for 2 to 4 weeks, with new lesions appearing as older ones heal. The progression from macules to scabs can be gradual, and the severity of the rash may vary among individuals.
Severe Cases
While most Monkeypox cases are mild, severe instances can occur, especially in individuals with weakened immune systems, children, and pregnant women. Complications may include secondary bacterial infections, respiratory distress, or eye infections, which can lead to vision impairment.
Diagnosis of Mpox
Clinical Diagnosis
Doctors diagnose Monkeypox based on clinical presentation and patient history. Key indicators include the presence of the characteristic rash and recent exposure to infected individuals or animals. However, relying solely on clinical signs may not be enough to confirm a diagnosis definitively.
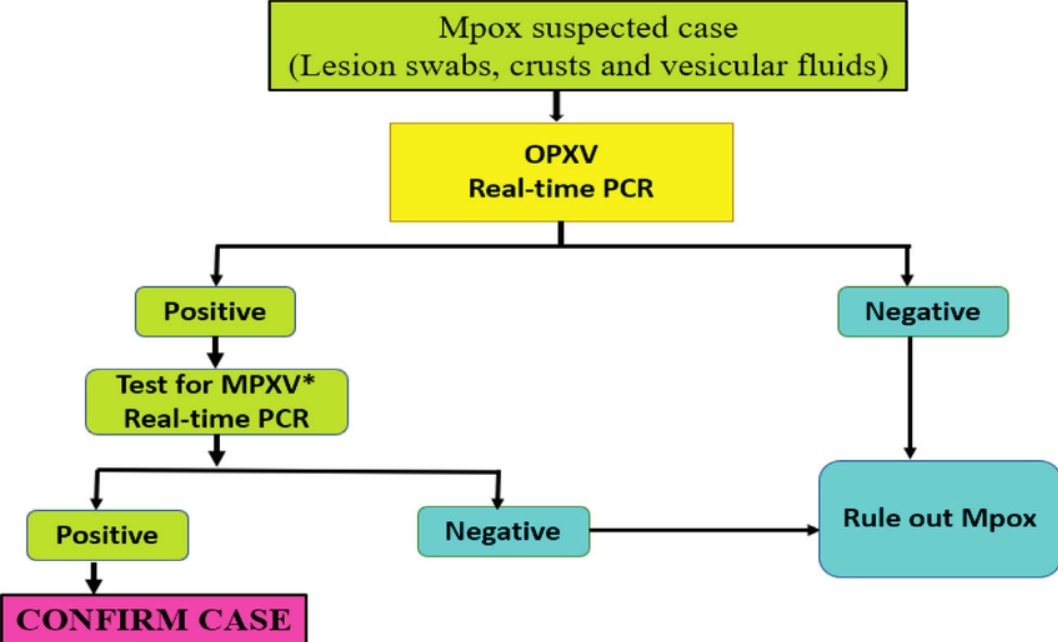
Laboratory Tests
Confirmatory diagnosis involves laboratory testing. Common tests include:
- Polymerase Chain Reaction (PCR): Detects viral DNA in lesions or bodily fluids.
- Serology: Identifies antibodies against the Monkeypox virus.
- Virus Isolation: Cultures the virus from patient samples.
These tests help differentiate Monkeypox from other pox-like illnesses and confirm the presence of the virus.
Differential Diagnosis
Mpox symptoms overlap with other diseases such as smallpox, chickenpox, and herpes simplex virus infections. Distinguishing Mpox from these conditions requires careful evaluation and laboratory confirmation.
Treatment of Mpox
General Management
Most Mpox cases are self-limiting, meaning they resolve on their own without specific antiviral treatment. The primary focus of management is to relieving symptoms and prevent potential complications:
- Rest: Getting sufficient rest is crucial to support the body’s recovery process.
- Hydration: Drinking fluids to maintain hydration.
- Symptom Relief: Using over-the-counter medications to manage fever, pain, and itching.
Antiviral Treatments
In severe cases or for individuals at high risk of complications, antiviral medications may be prescribed. Drugs such as tecovirimat (TPOXX) and brincidofovir are under investigation for their effectiveness against Monkeypox. These medications may help reduce the severity and duration of symptoms.
Supportive Care
Hospitalization may be required for severe cases to provide intensive care and monitor complications. Supportive care includes:
- Wound Care: Managing skin lesions to prevent infection.
- Respiratory Support: Providing assistance if breathing difficulties arise.
- Nutritional Support: Ensuring adequate nutrition and hydration.
Experimental Treatments
Research into Monkeypox is ongoing, with trials exploring new treatments and vaccines. Participation in clinical trials may offer access to cutting-edge therapies and contribute to advancing medical knowledge.
Prevention of Mpox
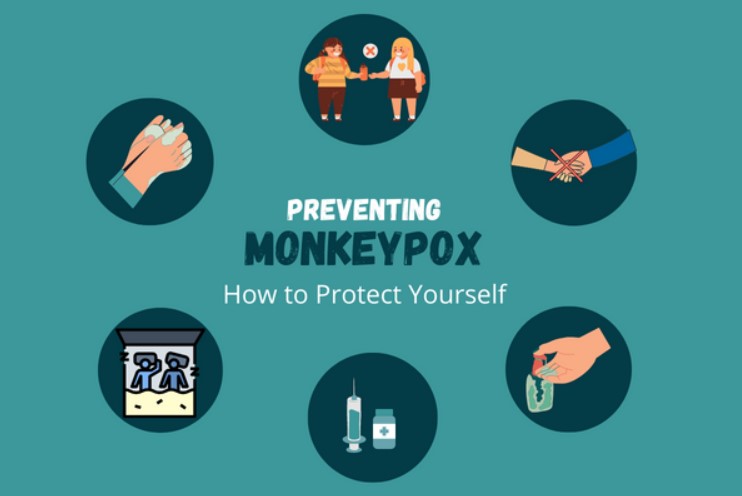
Vaccination
Vaccination is a key strategy for preventing Monkeypox, especially in high-risk areas. The smallpox vaccine has shown cross-protection against Monkeypox due to the similarities between the two viruses. New vaccines specifically designed to target Mpox are currently under development.
Hygiene and Sanitation
Good hygiene practices are essential for preventing the spread of Monkeypox:
- Handwashing: Regularly washing hands with soap and water, especially after contact with potentially contaminated materials.
- Sanitizing Surfaces: Disinfecting surfaces and objects that may have been in contact with infected individuals or animals.
Avoiding Exposure
Reducing exposure to Monkeypox involves several practical steps:
- Avoiding Contact with Infected Individuals: Staying away from people who show symptoms of Mpox.
- Handling Animals Safely: Using protective equipment and practicing good hygiene when interacting with animals in endemic regions.
- Safe Food Practices: Cooking meat thoroughly and avoiding consumption of raw or undercooked animal products. Also, try to keep yourself healthy and fit with yoga and exercises.
Public Health Measures
Public health initiatives play a crucial role in controlling Monkeypox outbreaks:
- Quarantine: Separating individuals who are infected to prevent the spread of the virus to others.
- Contact Tracing: Tracking and observing individuals who have been exposed to someone diagnosed with Mpox to prevent further spread of the disease.
- Awareness Campaigns: Educating communities about Mpox and preventive measures.
Mpox in Different Populations
Children
Children are more vulnerable to severe outcomes from Mpox due to their developing immune systems. Special care and attention are needed for pediatric cases, including vaccination and symptom management.
Immunocompromised Individuals
People with compromised immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk for severe Mpox. They require careful monitoring and may benefit from antiviral treatments.
Pregnant Women
Pregnant women are at risk of complications, including potential harm to the fetus. Pregnant individuals with Mpox should receive close medical supervision and may need tailored management strategies.
Geographic Considerations
Mpox is primarily endemic in Central and West Africa, where it is transmitted from animals to humans. Travel to these regions or contact with individuals from these areas can increase the risk of infection. Awareness and preventive measures are crucial for travelers and those living in or visiting endemic regions.
Current Status and Research
Recent Outbreaks
Recent outbreaks of Monkeypox have drawn global attention, with cases reported in countries outside the traditional endemic regions. These outbreaks highlight the importance of surveillance, timely response, and international cooperation to control the spread of the virus.
Ongoing Research
Research into Mpox continues to evolve, focusing on developing effective vaccines, treatments, and diagnostic tools. Scientists are exploring new antiviral drugs, improved vaccine formulations, and better understanding of the virus’s transmission dynamics.
Conclusion
Mpox is a serious disease with distinct symptoms and transmission methods. Understanding the causes, recognizing the symptoms, and knowing the available treatment options are essential for managing and preventing Mpox. By following preventive measures and staying informed about the latest research, individuals can contribute to controlling the spread of this disease and protecting public health.
FAQs
1. Can Mpox be prevented by vaccination?
Yes, vaccination with the smallpox vaccine or new Mpox-specific vaccines can help prevent Monkeypox.
2. How long does it take to recover from Mpox?
Most people recover within 2 to 4 weeks. Severe cases may take longer and require medical attention.
3. Are there any specific treatments for Mpox?
Treatment generally involves supportive care and antiviral medications for severe cases. Research into new treatments is ongoing.
4. What should I do if I suspect I have Mpox?
Seek medical attention promptly for diagnosis and treatment. Minimize close contact with others to reduce the risk of transmitting the virus.